Introduction
Lung cancer is one of the most common cancers in China. Its clinical manifestations are complex. It can be broadly grouped into four categories: symptoms of primary cancer, symptoms of intrathoracic spread, symptoms of distant spread and extrapulmonary manifestations. Symptoms and signs are accompanied with the site of occurrence, cancer size, pathological type, metastasis, and so on. Common symptoms are cough, hemoptysis or bloody sputum, chest pain, chest tightness, and others. Some patients manifest symptoms of shortness of breath, wheezing, and localized pneumonia due to airway obstruction.
The main treatments are surgery, radiotherapy, and chemotherapy, but no matter which treatment is used the treatment efficiency is not satisfactory. As a result, integrative treatment is of paramount importance. A wide range of thermal methods can be applied to the treatment of lung cancer; but whether it is interstitial coagulation hyperthermia or out-of-body heating, when used alone it is difficult to form an effective treatment temperature. Generally, radiotherapy or chemotherapy is combined.
Treatments
1. Surgery
Non-small cell lung cancer patients at phase I, II, or IIIa; patients with no clear surgical contraindications; and patients with clear indications for surgery can choose to have surgical treatment. Patients who are not suitable for surgery can select cryosurgery, radio-frequency ablation, or some other minimally invasive treatment.
2.Radiotherapy
Small cell undifferentiated carcinoma is the most sensitive to radiotherapy among the various types of lung cancers, followed by squamous cell carcinoma and adenocarcinoma. It is commonly used for patients with a wide range of diseases, with distant metastasis or a bad general condition, or not suitable for surgical treatment to improve symptoms and prolong life. Comprehensive application of radiotherapy can also be adopted with surgery. According to the location and extent of the cancer source as well as the expected difficulty of surgery, preoperative radiotherapy can improve the resection rate. If small cell undifferentiated carcinoma patients are suitable for surgical resection, preoperative radiotherapy can improve efficacy. For patients with lymph node metastasis and positive surgical margins, radiotherapy has a positive meaning. For patients who are unresectable due to old age or poor cardiac function, radiotherapy alone can be considered. For patients at phase IIIb who are not suitable for surgery due to existing mediastinal vital organ invasion or supraclavicular lymph node metastasis, radiotherapy; chemotherapy; or a comprehensive treatment of radiotherapy, chemotherapy, and hyperthermia can be conducted according to the pathology. Local conformal radiotherapy is safer because it improves the efficiency of the target dose. As a result, conformal radiotherapy technology is preferred for radiotherapy. The application of preventative brain radiotherapy for small cell lung cancer can reduce the number of brain metastases or delay brain metastases.
3.Chemotherapy
Small cell undifferentiated lung cancer is the most sensitive to chemotherapy among the various types of lung cancers and the efficacy is the best, followed by squamous cell carcinoma. Adenocarcinoma has the lowest sensitivity. In recent years, several drugs that act at different cell cycles are chosen for combination application. Anticancer perfusion for preoperative bronchial artery intubation can also reduce the cancer source and increase the resection rate. Postoperative chemotherapy is routinely given. Whole-body hyperthermia and local hyperthermia are applied according to the situation after hyperthermia assessment. Chemotherapy commonly uses a combination program. Postoperative chemotherapy is given for small cell lung cancer and non–small cell lung cancer except for phase Ia, and radiotherapy is given to patients with postoperative residues.
4.Hyperthermia
A wide range of thermal methods can be applied to the treatment of lung cancers, including whole-body hyperthermia; regional hyperthermia; interstitial coagulation hyperthermia; RF local hyperthermia; thermochemotherapy; thermoradiotherapy; combination of hyperthermia, radiotherapy, and chemotherapy; and intrapleural perfusion hyperthermic chemotherapy. Hyperthermia has the effect of enhancing chemoradiotherapy, the effect of using high temperatures to kill cancer cells, and the effect of promoting cancer immunity. Temperatures above 60°C can make the lung cancer tissue inactive in situ. Clinical studies have shown that hyperthermia has some therapeutic effect in advanced lung cancer; intrapleural perfusion hyperthermic chemotherapy has a better palliative treatment effect; and the combination treatment of radiotherapy, chemotherapy, and hyperthermia has some effect in patients with recurrence after radiotherapy.
5.Chelation Detoxification Therapy
Chelation detoxification therapy can be given, from the period of operation to chemotherapy, to the patient with physical weakness and low immunity after operation. On the one hand, it promotes physical recovery and regulates the immune system and, on the other hand, it can kill residual tumor cells or inhibit early metastasis.
6.Medical Ozone Therapy
For medical ozone therapy, EBOO is the preferred treatment, which is to be applied once every other day. At the same time, medical ozone acupoint injection is given. If the physical condition cannot tolerate EBOO, intravenous medical ozone saline, major autohemotherapy, minor autohemotherapy, and so on can be used. If the physical condition is weak and cannot tolerate EBOO, intravenous medical ozone saline or oxygen autohemotherapy can be chosen.
7. Traditional Chinese Medicine
The following syndromes are commonly seen at the early stage. For yin deficiency and internal heat, the prescriptions recommended are Shashen Maidong Decoction combining modified Baihe Gujin Decoction. For the syndrome of qi stagnation and blood stasis, the prescriptions recommended are Taohong Siwu Decoction combining modified Wuling Powder. Syndromes for the medium-advanced stage are commonly seen as follows. For the syndrome of turbid phlegm obstructing lung, the prescriptions recommended are Daotan Decoction plus Tingli Dazao Xiefei Decoction. For the syndrome of deficiency of lung–spleen qi, the prescription recommended is modified Xiangsha Liujunzi Decoction. For the syndrome of spleen and kidney deficiency, the prescription recommended is Lizhong Decoction combining modified Shishen Pill.
8.Acupuncture
8.1 Early lung cancer
Early lung cancer usually presents an excess of syndromes. The therapeutic principle should focus on eliminating pathogens and resolving mass as well as dispersing lung qi and dissipating phlegm.
8.2 Lung cancer at medium-advanced stage
Lung cancer at the medium-advanced stage mainly presents the syndrome of retention of phlegm heat in the lung or qi stagnation, and blood stasis. The therapeutic principle is to clear away heat and toxic substances, as well as resolve phlegm and soften hard mass.
9. Medicated Diet, Nutrition, and so on
It is recommended to give total parenteral nutrition the day before thermochemotherapy. Then, mainly adopt oral medicated diet and supplementary nutrients. Pay attention to chemotherapy-induced gastrointestinal side effects. In addition to the adjustment of TCM, apply appropriate vitamins, minerals, and other elements. Nutrition is an important treatment factor for medium-advanced lung cancer. Enough nutrients also need to be included in addition to the necessary medicated diet conditioning. If necessary, total parenteral nutrition is given. At the same time, pay attention to psychological counseling, qigong, sports, music, and other therapies to keep the patient calm, positive, and optimistic as well as to improve the self-healing ability. Encourage patients to continue their daily living in spite of their affliction.
10.Others
The prognosis of most patients at the early stage is acceptable. Patients at the medium-advanced stage have a predicted period of survival. Give appropriate psychological counseling to patients to reduce their psychological fear of cancer, and recommend them to practice qigong. Adhering to proper exercise can help patients recover faster.
Typical Case
69 years old male patient, was admitted to Clifford Hospital for “space-occupying”lesion in the left upper lobe of the lung with cough and hemoptysis for 6 days. Patient had symptoms of fever, cough, expectoration, and excessive blood-tinged sputum for six days before admission to hospital. He was given anti-infection therapy from a local hospital (specific drugs were unknown). Chest X-ray and CT scan revealed space-occupying lesions in the left upper lung. Lung cancer and obstructive pneumonia were considered. After treatment, patient’s fever had stopped, cough and expectoration decreased. Patient was then transferred to Clifford Hospital for further treatment.
Past medical history: the patient had a history of hypertension and took a hypotensor for treatment. At the time of admission, his blood pressure was stable. The patient was hospitalized at Clifford Hospital due to cerebral infraction and discharged in March 2009 when the condition improved. Patient had an 8-year history of diabetes and took oral Repaglinide and Glucophage for treatment. He had been a 2 pack a day smoker for many years and finally quit smoking 3 years ago. There was no history of hepatitis, tuberculosis and heart disease.
Patient was in good mental condition, with hoarseness, herpes around the lips, cough, sputum and some sputum tinged with a small amount of blood. Patient had good appetite and did not have wheezing, chest tightness and other discomfort. Patient had pink tongue, thin white fur, thready and weak pulse.
Physical examination: Barrel chest and thoracic symmetry. Breathing sounds at the left upper lung with percussive flatness were not detected by auscultation. A few fine, thin, and moist rales could be heard at the left lower lung. Breathing sounds were clear at the right lung, wet and dry rales not being heard. There was no uplift in the precordium. The apex beat was at the left fifth interspace and about 2cm inside the central line of collarbone. The border of cardiac dullness was normal. Heart rate was 94 beats/min, with regular rhythm. Pathological murmur was not heard in each cardiac valve area. The KPS (Karnofsky performance score) was 90.
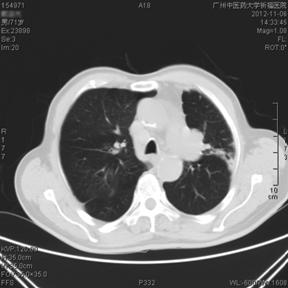
Auxiliary examination: CT: (1) Space-occupying lesion in the left upper lung was considered to be a possibility of lung cancer; other symptoms were supraclavicular fossa, mediastinal lymph node metastasis, pericardial effusion, and a small amount of left pleural effusion. Biopsy with tracheoscopy was recommended. (2) Obsolete lacunar lesions were at the left basal ganglia and the left thalamus. Fiber-optic bronchoscopy: left lung cancer. Pathology report: squamous cell carcinoma.
Laboratory tests: Blood routine: RBC 3.74×1012/L, Hb 102g/L,WBC 11.00×109/L, N 82.4% and PLT 549×109/L; Blood biochemistry: ALT 47 U/L, AST 33U/L,TP 60.5 g/L,ALB 34.0g/L,ALP 215U/L,GGT 87 U/L,TBIL 12.2 umol/L, DBIL 34.5 umol/L, Cr 99 umol/L, Ua 277 umol/L, GLU 7.01 mmol/L, TG 1.13 mmol/L, GHO 2.85 mmol/L, K+ 3.97 mmol/L, Na+ 140.90 mmol/L, Cl- 103.80 mmol/L, and Ca2+ 2.09 mmol/L. The five tumor markers were as follows: CEA: 3.93ng/ml, CA15-3: 6.06 U/ml, TPSA: 2.81ng/ml, CA19-9: 19.38 U/ml and AFP: 0.61ng/ml. The remainder was normal.
Diagnosis: left lung squamous cell carcinoma and multiple lymph node metastasis (T3N3M0, stage Ⅲb)
Integrative treatment prescription: Patient refused chemotherapy; as a result, TCM, acupuncture, detoxification, hyperthermia, medical ozone and other integrative treatment were given. The patient was with Yin deficiency and phlegm-heat, as well as a complication of deficiency and excess of vital Qi and etiological factors. The principle of TCM was to nourish Yin and clear away lung heat, reduce phlegm, and resolve masses.
Medications: Modified Qingjin Sanjie Decoction was given. The specific medication: Gecko 6g, Semen Coicis 30g, Agrimonia Pilosa Ledeb 30g, Prunella Vulgaris 15g, Platycodon Grandiflorum 12g, Fritillaria thunbergii Miq 15g, Polyporus Umbellatus 20g, Radix Adenophorae 30g, Ophiopogon Japonicus 15g, Carapax Trionycis 30g, Radix Rehmanniae 20g, and Schisandra Chinensis 10g, one dose a day and decocted it with water for oral dose.
Acupuncture on acupoints: took Feishu, Zhongfu, Chize, Zusanli, Quchi, Fenglong, Xuehai, Taichong, Linggu, Dabai and Waisanguan. Even reinforcing-reducing method was used for acupuncture. Retained the needle for 20 minutes, once per day. Took 2 days off after five times of acupuncture.
Moxibustion on acupoints: Feishu, Dazui, Guanyuan and Zusanli. Took two points each time and conducted moxibustion for 10 minutes per point, once per day. Took 2 days off after five times of moxibustion.
Auricular acupoints: Lung, Chest, Subcortex, Shenmen, Trachea, Endocrine and Jiaogan. Methods: stuck auricular points with cowherb seed. The patient was asked to press by himself 3-5 times every day , with 3-5 minutes for each point, twice a week, alternating ears.
At the same time, a combination of parenteral nutrition with medicated diet conditioning to strengthen supportive treatment was conducted; local hyperthermia of chest three times a week, and chelation detoxification three times a week, simultaneously with hyperthermia. The medical ozone therapy selected was EBOO, twice a week. It was conducted at the intervals of hyperthermia. After 1 month of hospitalization, patient had improved and was discharged. After a 1-week break, patient returned to the hospital for treatment.
Treatment outcome: after 1 month of treatment in hospital, the patient’s general condition had improved significantly. Cough and hemoptysis had gradually reduced. Speech was clearer than before. Weight gain was 3kg. Diet, urine and stool were basically normal. The KPS was 100. The patient adhered to treatment as an outpatient and by intermittent hospitalization. In the 2-year follow-up after being discharged from hospital, the patient was in recovery. Lung CT was reviewed 10 months and 22 months after treatment, the lesions were significantly reduced and in stable condition. The patient is still being followed up now (Fig. 1, Fig. 2, Fig. 3).
 Fig. 1 Before Treatments: October, 2010, CT.BMP
Fig. 1 Before Treatments: October, 2010, CT.BMP

Fig. 2 After Treatments: April, 2011, CT.BMP
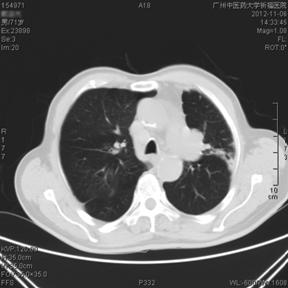
Fig. 3 After Treatments: November, 2011, CT.BMP